guides & resources
Special Enrollment Period Guide for Administrators
Here’s everything you need to know about Special Enrollment Periods (SEP) as a decision-maker at your organization.

Overview
What is a Special Enrollment Period (SEP)?
An SEP, or Special Enrollment Period, represents a span of time outside of the annual Open Enrollment Period (which takes place from November 1-December 15) and provides an opportunity for individuals to select new individual health insurance plans mid-year.
Jump to a section in the guide
Overview: What Is An SEP for Health Insurance?
Utilize your chance to change plans mid-year.
As you have explored healthcare options for your team, you may have wondered, “what is an SEP for health insurance?” An SEP, or special enrollment period, represents a span of time outside of the annual Open Enrollment Period. Open Enrollment takes place from November 1-December 15 and provides an opportunity for individuals to select new individual health insurance plans for the calendar year.
After Open Enrollment ends, individuals can only change plans if they qualify for a special enrollment period (SEP). It’s important to note that an SEP applies solely to individual health insurance plans that are purchased through the Health Insurance Marketplace. In order for your employees to take advantage of an SEP, there are many unique factors that must be considered.
What Makes Your employees Qualified for an SEP?
Five primary factors qualify you for an SEP.
There are five primary life changes that can qualify your employees for an SEP. These life events include loss of qualifying healthcare coverage, change in household size or primary place of living, change in Marketplace eligibility, and error in enrollment or health plan.
Let’s examine real-life examples of these events to better understand the qualifications for an SEP.
1. Loss of Qualifying Healthcare Coverage
An employee can lose their healthcare coverage for a variety of reasons. Job loss, whether it is voluntary or involuntary, may qualify an individual for an SEP because it would mean the employee no longer has access to the employer-sponsored health plan. Loss of healthcare coverage can also be represented through an employer no longer offering employee healthcare or switching to providing coverage that is not considered qualifying coverage. According to HealthCare.gov, an individual may only be eligible for an SEP if they or someone in their household has lost coverage in the past 60 days or expects to lose coverage in the next 60 days.
2. Change in Household Size
Another factor that may qualify an individual for an SEP is a change in household size. Major life events such as:
- marriage
- death of a family member
- having a baby
- adopting a child
- placing a child in foster care
- or changes surrounding child support/court orders
These factors are all considered changes that may qualify an employee to select new individual plans.
3. Change in Primary Place of Living
If an employee has recently moved, applying for an SEP could be beneficial for you and your household! Permanently moving to a different county or an area with a different ZIP code is a life change that could qualify an individual for an SEP. Other living changes such as moving during seasonal employment, moving to the United States from a different country, moving to where your school is located, or moving from transitional housing are also considered changes in a primary place of living. Just keep in mind that vacations and moving for medical treatments are not qualifying events.
4. Change in Eligibility for Marketplace Coverage or Help Paying for Coverage
This event occurs when an individual is newly eligible or ineligible to pay for healthcare coverage. Many factors such as moving, becoming an American citizen, being released from incarceration, or becoming a member of a federally recognized tribe may lead them to qualify for an SEP in this way.
5. Enrollment or Plan Error
Although this occurrence is extremely rare, if your employee believes that there was an error during the enrollment and plan selection process through the Health Insurance Marketplace, they may be eligible for an SEP. Enrollment or plan error can look like not being enrolled in a plan or mistakenly being enrolled in a different plan. These issues can be attributed to misinformation or technical errors, and it is crucial to inform the Marketplace if they were enrolled in the wrong plan.
What Kind of Plan Can your employees Get During a Special Enrollment Period?
Qualify for individual health insurance.
The advantage of qualifying for a special enrollment period is that your employees get to enroll in a new individual health insurance plan through the Health Insurance Marketplace. The Health Insurance Marketplace is located at HealthCare.gov and allows individuals to shop for the individual health insurance plan that best fits their needs! As a Remodel Health customer, we will help guide you through the process of selecting a plan. With individual health insurance, your organization can choose a budget-friendly plan that provides excellent coverage.
Example Scenario: Julie is eligible for an ICHRA.
Therefore, Julie must enroll in a new individual plan by August 29.
Example Scenario: Mark is on his Spouse’s Plan.
An SEP does not occur, although Mark can not enroll in a Marketplace plan, there are other options available until Open Enrollment. An advisor can help him review his options.
How Do employees Apply for an SEP?
Apply for an SEP online.
If one of your employees believe they meet the qualifications for an SEP and are ready to select a new plan, it’s time to apply! First, they need to visit this link to answer a few quick questions and complete the Marketplace application. Then, if they meet the qualifications, they will be able to view plan options and prices. This application is an important step in notifying the Marketplace about their eligibility for an SEP. If they do not complete the application, the Marketplace will not be aware of their desire to utilize a special enrollment period and they will not be able to enroll in a new plan until the next annual Open Enrollment period.
What Documents Do your employees Need for a Special Enrollment Period?
Submit all relevant documentation.
After applying for an SEP, your employees may need to submit documents to confirm their eligibility. The required documentation that needs to be submitted to HealthCare.gov is dependent on individuals’ specific circumstances. For example, if an employee recently changed their primary place of living, they may have to submit bills or mortgage documents that include their name and the date they moved. Thankfully, Remodel Health’s team of experts are able to help with the process of submitting required documentation.
How Long Is a Special Enrollment Period?
Apply on time for your SEP.
Most SEPs are either 60 days before or 60 days after the specific qualifying life event occurs. However, job-based plans must provide a minimum SEP of 30 days. If your state of residence runs its own Health Insurance Marketplace, there may be different Special Enrollment Periods. In order to avoid uninsured employees, it’s important to know exactly how much time they have to choose their new plan. To find out more information about an SEP, contact your Remodel Health Customer Success Representative at [email protected].
Example Scenario: Elizabeth’s SEP Length.
Elizabeth has an SEP for 60 days and must be enrolled in a Marketplace plan by July 30.
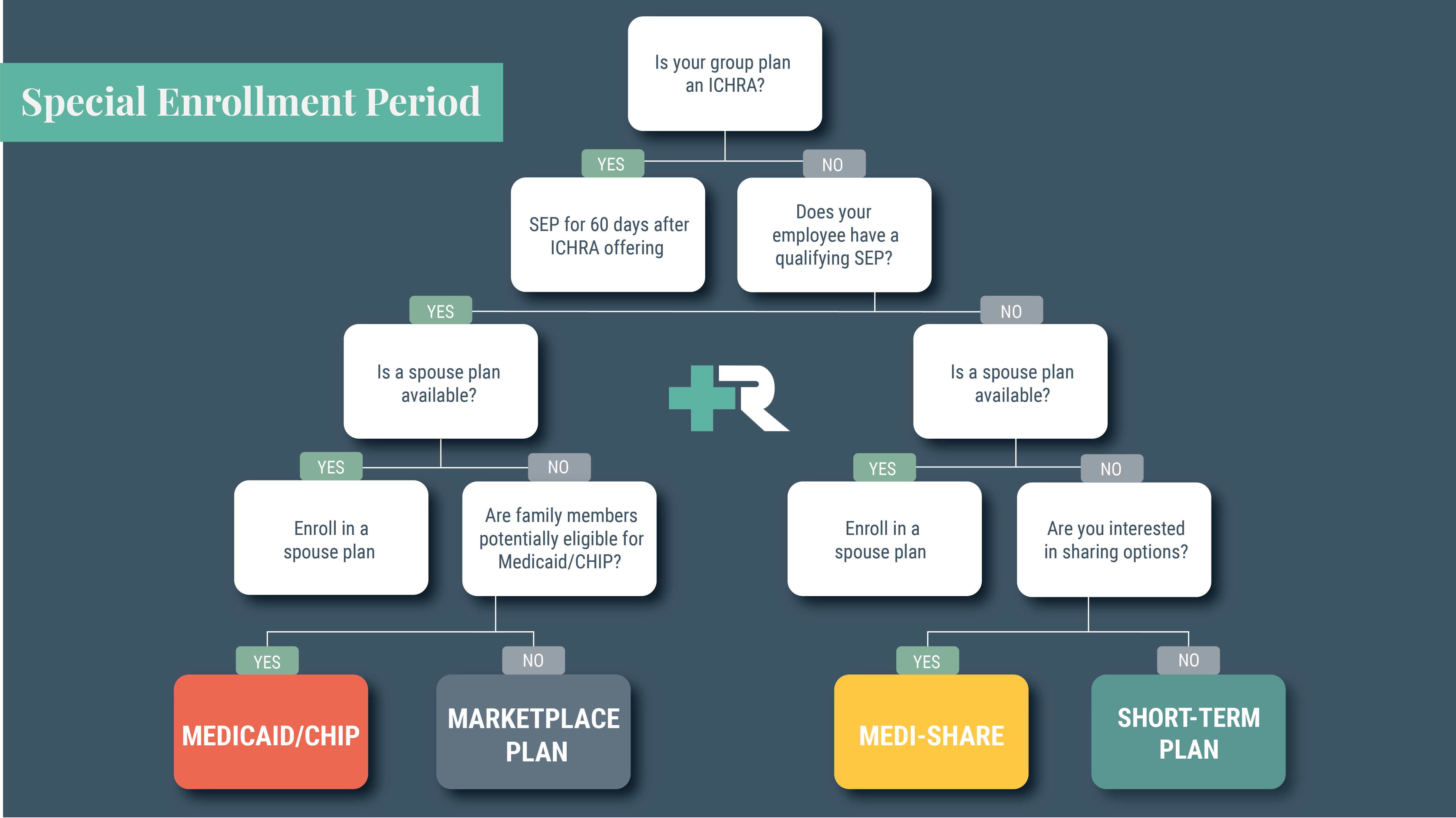
Your employee Didn't Qualify for an sEP. What’s Next?
Appeal the outcome or wait for Open Enrollment.
If your employee applied for an SEP and the Marketplace determined that they were not eligible, they can file an appeal. The employee will have 90 days to file this appeal and request reconsideration. If they decide not to appeal this decision, they will have the opportunity to enroll in an ACA-compliant plan during Open Enrollment. Not being eligible for an SEP may feel discouraging, but thankfully, they have options to make sure their healthcare coverage is secured.
Example Scenario: Joel is Uninsured and Didn’t Qualify for an SEP.
Although an SEP does not occur, while Joel can not enroll in a Marketplace plan, there are other options available until Open Enrollment. An advisor can help him review his options.
How Do I Cancel My Organization's Current Plan?
Individual insurance allows you to cancel at any time.
If your organization is currently enrolled in a traditional group health insurance, you can only cancel your plan during the Open Enrollment period. However, if you have individual health insurance through the Marketplace, you can cancel your plan at any time! This is just one of the many benefits and conveniences of switching to individual plans!
Canceling an individual health insurance plan is as simple as logging into your account or calling the Marketplace to inform them of your decision.
Get in touch with our team of experts.
Get in touch with our team of licensed experts.
Do you have questions about SEPs, the Marketplace, or enrolling your organization in a new individual health insurance plan? We are here to help and guide you every step of the way! Our licensed experts can help you find the best plan and navigate the complex world of healthcare. With Remodel Health’s proprietary health benefits software, you can also easily manage your employees’ individual health insurance. The key benefits of our software include tax calculations, shopping and enrollment assistance, year-round support, and so much more.
Connect with us or contact our Care team at [email protected] to learn how to improve your health benefits and experience the freedom of individual health insurance!
on the blog
Expert insights at your fingertips.
Check out our resource library for easy-to-read blogs, videos, guides to big topics, case studies, and more!



